The World Health Organisation Director-General Tedros Adhanom Ghebreyesus says “2022 must be the end of the COVID-19 pandemic”. He is hopeful it will be because after two years, “we know the virus very well, and we have all the tools [to fight it]”.
Similarly, The Economist, in a recent article, wrote:
“COVID is not done yet. But by 2023, it will no longer be a life-threatening disease. It will still pose a deadly danger to billions in the poor world, [but] will be well on the way to becoming just another disease”.
Whatever the answer is, 2022 will be the year we finally have all the means, measures, and tools to control the pandemic to a non-lethal state.
Some 3.8 billion have had at least one COVID jab, and 2.8 billion are fully vaccinated. Together with those who have acquired the disease, half the world’s population has had some level of immunity. Eventually, COVID-19 will become endemic: the transmission will remain steady, following seasonal patterns, with fewer spikes in infection.
In an ideal situation, the harm caused may end up somewhere between influenza, which kills an estimated 300,000 to 650,000 people annually, and other coronaviruses, such as the common cold.
Vaccine equity is a global problem
But endemicity is still a long way off for many countries. The virus will continue to affect our lives and livelihoods unless the global community collectively addresses inequitable access to vaccines, therapeutic agents and diagnostics.
If we don’t address this quickly enough, our exit from the pandemic will be set back, possibly for months or years.

Current vaccines by themselves are insufficient to stem transmission. Increases in cases should continue to be expected whenever public health and social measures are lifted, irrespective of vaccination coverage.
Currently, we are giving the virus the room it needs to thrive through uneven and inconsistent national policies undermined by division and politics.
Of the more than seven billion doses administered so far, less than 3% have been in countries on the African continent. The failure to provide sufficient vaccine doses to low and middle-income countries is unethical and economically unwise.
SARS-CoV-2 has shown its ability to better adapt to the human host, with variants Alpha and Delta demonstrating enhanced transmissibility throughout the pandemic.
One of the biggest unknowns in 2022 will be how this evolution continues. Delta continues to evolve, and the Omicron variant has shown that the virus will continue to adapt.
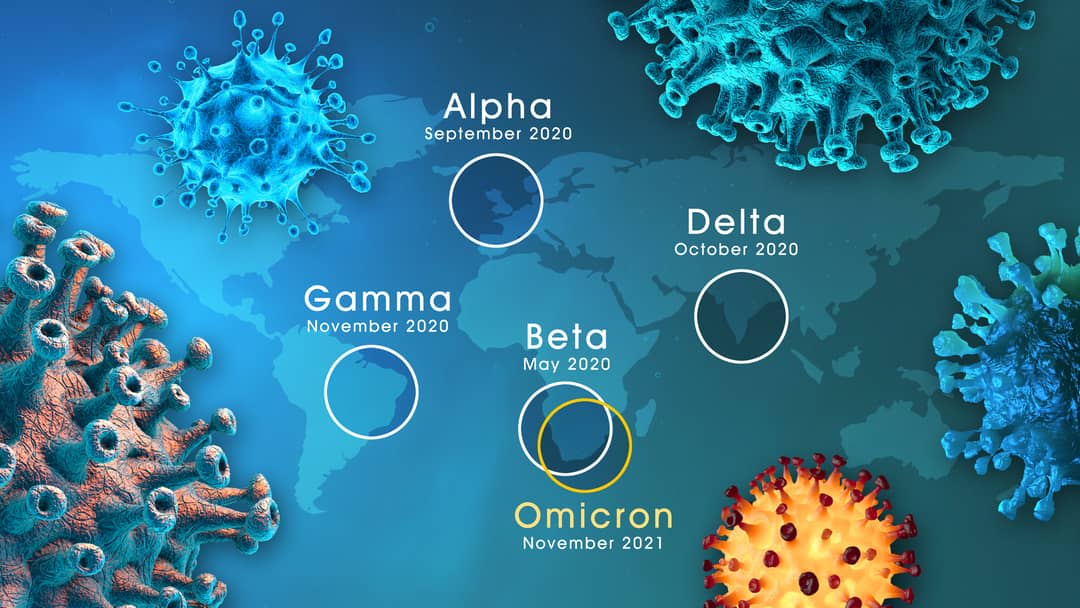
Viruses mutate because they’re constantly making copies of themselves in enormous numbers. Each time it is transmitted from one person to another, the chances of making errors (mutation) are high.
Think of it this way. Suppose you are typing exceptionally fast multiple times. You’d probably make some errors. This is precisely how the virus mutates. The longer the pandemic rages on, the more chances the virus will evolve, especially in unvaccinated individuals.
Studies have shown that humans are exposed to all four coronaviruses between the ages of three and five. These initial infections lay the foundation for the body’s future immune response. As new variants of the endemic coronaviruses naturally evolve, the immune system will have a head start in fighting them off — not enough to eradicate the virus instantly, but enough to ensure that symptoms don’t progress much beyond the sniffles.
Past studies clarify that partial immunity can keep people from getting seriously ill, even as coronaviruses successfully enter their systems.
While initial data shows that protection from booster doses might wane after 10 weeks, this is merely looking at the efficacy of neutralising antibodies. However, neutralising antibodies are not the only defence that the immune system can muster. Immune responses are layered and redundant; where one-layer falters, another can swoop in to help.
Killer T-cells represent one such layer. Their modus operandi comes with an alternative. They home in on different aspects of the virus than antibodies do.
Data from Alessandro Sette’s lab, an immunologist at the La Jolla Institute for Immunology, and Andrew Redd of the National Institutes of Health, showed that despite Omicron’s many mutations, most protein fragments recognised by T-cells are identical to those of other variants.
These findings suggest that T-cells trained by vaccines or previous infections will respond aggressively to Omicron rather than standing by. In addition, all vaccines generate memory B-cells, which produce high levels of neutralising antibodies if they see the virus or its variants again. Memory B-cells, once generated, are long-lasting, and this is observed in all vaccinated individuals despite the threat from Omicron.
We have endured two years of missed opportunities, missed education, missed connections with family and loved ones. Without action, 2022 could be the same.
Countries need to effectively scale and make available new oral therapeutics with the potential to reduce the chance of progression to severe disease. Evidence is accumulating that booster doses are significant for protecting against the Omicron variant; accelerating their rollout will help protect populations. Given public fatigue and the lessons of the past two years, finding the right combination of public-health measures will be critical.
While evidence has suggested that Omicron may lead to more frequent hospitalisation in children than other variants, some early findings have pointed toward a mild clinical course.
According to a recent study from South Africa, people infected with Omicron may have increased immune protection against Delta. If Omicron displaces Delta and proves milder than past variants, it would reduce the incidence of severe COVID-19 disease.
Sticking to the health measures
Our primary goal is to slow down virus spread by adhering to existing hygiene measures and speeding up the vaccination (which now has to include booster doses at all age groups).
We know that variant-specific boosters are currently in the pipeline for various vaccine manufacturers, which can be part of the booster dose regiment in the future.
With newer variants having immune evading capabilities, we will continue to see a slight increase in the number of cases. But what we should be looking at is the number of severe cases, hospitalisation rate, and mortality.
Looking ahead to Oral therapeutics
The clinical management of COVID-19 has come a long way since the early days of the pandemic. Recent results from Merck–Ridgeback Biotherapeutics and Pfizer on their oral drugs Molnupiravir and PAXLOVID, respectively (two antivirals, with different mechanisms of action), represent a material advancement and increase the chance that the impact of the Omicron variant can be controlled. In its final study, Pfizer reported that PAXLOVID reduced the risk of hospitalisation or death by about 89% for high-risk patients and about 70% for standard-risk patients.
Oral therapeutics that significantly reduce the chance of progression to severe disease after symptom onset may enable a higher fraction of cases to be managed as outpatients. Such therapies are also easier to administer in lower-resourced regions.
Although COVID-19 is seen as a disease that primarily affects the lungs, it can also damage many other organs, including the heart, kidneys and brain. Organ damage may lead to health complications that linger after COVID-19 illness. Some adults and children experience multisystem inflammatory syndrome after they have had COVID-19. In this condition, some organs and tissues become severely inflamed.
One good piece of advice is to get the booster doses, stay vigilant, and practice the hygiene protocols that we have become so used to.
This article was published by Lens.














