Coming back stronger
The COVID-19 crisis has turned a spotlight on existing health, social and economic inequities in Australia and internationally. Few have been left untouched by the direct and indirect effects of the global pandemic, and some have endured greater hardships than others.
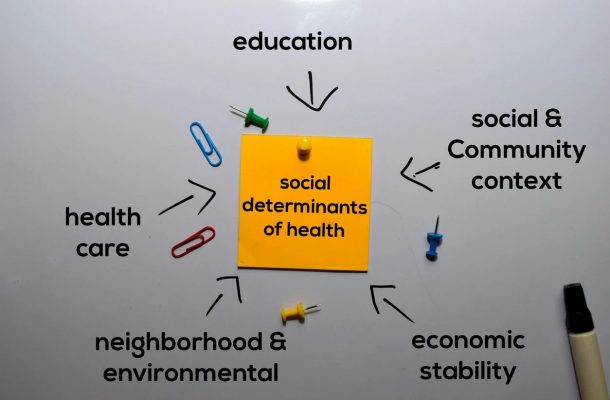
COVID-19 has been a stark reminder of the importance of the social determinants of health, and the need to prioritise support for marginalised individuals and groups in our community.
As of 14 September, 2020, 7.2 million people have been infected with COVID-19, and more than 927,000 people have died worldwide. In Australia, the total number of cases is more than 26,700, with more than 820 deaths.
People with pre-existing health conditions, and those from lower-socioeconomic communities and marginalised groups are at greater risk of experiencing the worst effects of the pandemic compared with those from non-marginalised communities.
When people contract COVID-19 and have pre-existing conditions such as heart disease, obesity and asthma, they’re more likely to experience respiratory failure and death.
The inequalities
The impacts of COVID-19 have not been evenly distributed. Respiratory infections such as COVID-19 are more easily transmitted among lower-socioeconomic communities who typically live in more crowded conditions.
People in such communities also experience greater repercussions from the pandemic due to higher levels of insecure work and heightened risk of poverty.
Culturally and linguistically diverse communities often have more difficulty accessing timely health-related information in a form they can understand.
Additionally, they’ve been more vulnerable to misleading rumours and confusing messages about coronavirus. In countries such as the US and UK, patients and health workers from racial/ethnic minorities are more likely to die from COVID-19 than those from ethnic majority communities.
The pandemic has also worsened inequality for women. This is due to greater job losses for women who hold mainly insecure, informal and low-paying jobs, heightened risk for female frontline workers and community volunteers, and increases in domestic violence.
Differing lockdown responses and uneven compensating policies have also contributed to increasing inequality between, and within, countries. The speed of transmission and need for a swift lockdown response to contain outbreaks limits time for consultation with affected communities.
As seen recently in the rapid lockdown of nine public housing towers in inner Melbourne, government responses to COVID-19 can risk increased social exclusion and stigmatisation at a time when communities need to work together.

COVID-19 has especially affected those caring for and treating older adult residents and patients. Care workers in residential aged care, professional nurses and medical practitioners in inpatient care settings are at heightened risk of infection themselves.
Care workers’ options for safe employment in residential aged care have to date been limited by the lack of knowledge and skill in relation to personal protective equipment use.
The safety of care workers and aged care residents has been significantly compounded by the casualisation of this workforce and low rates of pay, where care workers work across facilities and unwittingly spread COVID-19.
Health and health equity matter now more than ever
Research conducted by the World Health Organisation identified that up to at least 80% of health outcomes are attributed to the social determinants of health.
Social determinants refer to the conditions in which we are born, grow, live, work and age – thus the impact of the pandemic will depend on how our social and economic systems respond. Health depends on our access to quality healthcare as well as decent housing conditions, secure and safe employment conditions, socially inclusive communities, and more.
Even in wealthy countries such as Australia and Britain that have national health systems, health inequities persist. In Australia, Aboriginal and Torres Strait Islander child mortality rates are still twice the rate for non-Indigenous children.
In Britain, life expectancy has fallen in the most deprived communities, and the amount of time spent in poor health has increased in the past decade.
As the race for a COVID-19 vaccine continues, we must remember that our future health is also dependent on strong and equitable social, economic and environmental conditions.The long-term impacts of the pandemic may last for many years.
More urgent action is needed to address the social determinants of health and health inequities in order to ensure that the most marginalised and vulnerable in our community don’t suffer greater disproportionate effects from the pandemic.
A stronger future
We have an opportunity to rethink, reorient and reshape our society so everyone, regardless of their circumstances, is able to reach their full potential. A focus on strong communities is vital to ensure that everyone is living in optimal conditions and will be protected against COVID-19.
COVID-19 pandemic recovery for all means:
-
A well-funded health system and health sector, including primary healthcare and public health. This involves greater investment in prevention and health protection.
-
More action to reduce existing health inequities and vulnerabilities, which better prepares communities for public health crises, through:
-
improved public housing to reduce overcrowding
-
secure, safe and health workplaces for all
-
improved access to social and mental health supports and services
-
more funding for local community-led initiatives. For example, the Aboriginal and Torres Strait Islander community-led response has successfully emphasised health equity through all stages of the pandemic to ensure low rates of infection.
-
-
Improved quality of care and protection for care workers and residents in aged care through:
-
increased funding for permanent employment, and improved pay rates for care workers in residential aged care
-
improved education and training for care workers in residential aged care
-
professional nursing support for care workers in residential aged care.
-
-
If and when a vaccine for COVID-19 becomes available, wealthy nations need to step up and ensure that everyone, including those living in less privileged countries and circumstances, can access the vaccine and other treatments.

The COVID-19 pandemic has upended all of society. Life will likely never be the same again.
Government and community responses to the pandemic have also highlighted strengths and resilience in a time of adversity. It has also drawn attention to the need for greater efforts to protect individuals and communities who are most vulnerable to the pandemic.
Building stronger social and economic systems are paramount to support every individual, family and community to thrive and flourish. Doing so will honour the spirit of care and humanity shown by care workers in aged care and health practitioners across the health system, as well as those in other sectors.
Our recovery from the pandemic is ultimately dependent on strong communities. We are all in this together.
This article was written by Mandy Truong, a Research Fellow at Monash School of Nursing and Midwifery; and Jacqui Allen, a Senior Lecturer in Nursing and Midwifery.
Mandy is a public health researcher and health professional at Monash University. Her main research interests centre on health equity and the social determinants of health, specifically in relation to racism, discrimination and family violence.













